Low Rectal Cancer
Low Rectal Cancer Surgery
The diagnosis of low rectal cancer will most likely lead to surgery that will remove most of your rectum. Low rectal cancer, by definition, is located in the middle or lower section of your rectum. Because the surgeon will remove not only the cancerous section of the rectum but also a reasonable margin below and above the cancerous section,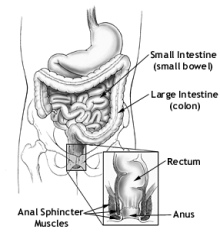 there will be very little left of your rectum after the surgery.
there will be very little left of your rectum after the surgery.
Low rectal cancer surgery has the potential for worse clinical outcomes than surgery for colon cancer. Quality of life, local recurrence and survival are generally worse after rectal cancer surgery. There is continuing debate about the extent of resection, the type of reconstruction, and the training of a rectal surgeon.
Operating on any section of the rectum is technically challenging for a surgeon. The rectum is surrounded by the pelvic skeletal structure. Historically, low rectal cancer required a colostomy because of the difficulty in cutting the rectum near the anal verge and then having to sew around the perimeter of the colon near the anal verge. There is simply very little room for a surgeon's hands to get into this area and sew a good suture around the perimeter.
I n the early 80's there was a technological breakthrough in dealing with low rectal cancer. A clever technician invented a stapling device that could be inserted through the anus and into the remaining rectum after the surgeon had cut the rectum near the anal verge. Instead of having to hand sew the perimeter, this invention simplified the task of connecting the colon to the small part of the rectum above the anal verge. This little invention solved the problem of how to quickly and permanently connect the stub end of the rectum to the colon in the limited area around the pelvic structure. The technique, called "end-to-end anastomosis", allowed many patients to avoid a colostomy. However, although this new technique solved a technical problem, it ignored the functional consequences of the removal of most of the rectum.
n the early 80's there was a technological breakthrough in dealing with low rectal cancer. A clever technician invented a stapling device that could be inserted through the anus and into the remaining rectum after the surgeon had cut the rectum near the anal verge. Instead of having to hand sew the perimeter, this invention simplified the task of connecting the colon to the small part of the rectum above the anal verge. This little invention solved the problem of how to quickly and permanently connect the stub end of the rectum to the colon in the limited area around the pelvic structure. The technique, called "end-to-end anastomosis", allowed many patients to avoid a colostomy. However, although this new technique solved a technical problem, it ignored the functional consequences of the removal of most of the rectum.
The rectum is not simply the "end of the colon". It serves as the reservoir that holds the stool until it is a convenient time to go to the toilet. Without a rectum you have immediate and constant urges when the stool contacts the sensitive nerves that surround the anus. Without the rectal muscles that can contract to empty the rectum when you relax the anal voluntary muscles, only a small amount of stool can be pushed into the toilet. Within a short time you may feel strong urges and have to again "get to the toilet" to avoid incontinence. This process continues until a "string of stool" has been emptied into the toilet.
T he consequences of the "end to end anastomosis" on bowel function led to the development of a new surgical technique that is called a "J Pouch". The goal of the "J-Pouch" technique is to create a "neo-rectum" that will simulate the natural rectal volume and hopefully the characteristics of the rectum that was removed. In the surgery, most of the rectum is removed and then a section of the colon is folded back onto itself. The surgeon first sews the end of the colon shut and then makes a long longitudinal cut along the side of the colon. This cut is then sewn together to make a reservoir for stool. At the end of the operation, the staple device is used to connect a hole cut in the "neo rectum" back to the stub of the remaining rectum. This surgery is more technically complicated than the "end to end anastomosis" but the bulk of the sewing can be done outside of the body cavity.
he consequences of the "end to end anastomosis" on bowel function led to the development of a new surgical technique that is called a "J Pouch". The goal of the "J-Pouch" technique is to create a "neo-rectum" that will simulate the natural rectal volume and hopefully the characteristics of the rectum that was removed. In the surgery, most of the rectum is removed and then a section of the colon is folded back onto itself. The surgeon first sews the end of the colon shut and then makes a long longitudinal cut along the side of the colon. This cut is then sewn together to make a reservoir for stool. At the end of the operation, the staple device is used to connect a hole cut in the "neo rectum" back to the stub of the remaining rectum. This surgery is more technically complicated than the "end to end anastomosis" but the bulk of the sewing can be done outside of the body cavity.
The construction of a "J-Pouch" requires a lot of sutures. These are self dissolving sutures that are not needed after the body has had a chance to naturally heal. Sutures are different than the stainless steel metal staples which do not dissolve and remain forever. To allow the body to heal it is necessary to allow the "neo rectum" to be inactive for a few months. To divert stool from the area of the "J-Pouch" it is necessary to construct a temporary colostomy. A colostomy is a surgery that cuts the colon well above the rectum and pulls the ends of the colon to the surface. Stool empties directly into the colostomy pouch in an uncontrolled manner.
After the rectum has healed, another operation is preformed to sew the two ends of the colon together and then push the reconnected colon back into the body cavity so that stool is again directed back to the rectum.
T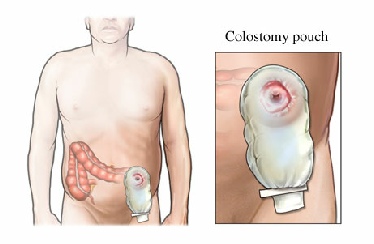 his very brief non-technical description of the history of surgical treatment for low rectal cancer is very important to understand before you decide which procedure you are willing to authorize. The more traditional "end to end stapled anastomosis" is a relatively simple operation. The healing time is much shorter than the "J pouch" procedures because there is no hand suturing and no need for a temporary colostomy. The quick healing of the wound also may facilitate the beginning of adjuvant therapy. In addition, you will not have to wear a colostomy bag for three to four months and then have to endure another major surgery to reverse the colostomy.
his very brief non-technical description of the history of surgical treatment for low rectal cancer is very important to understand before you decide which procedure you are willing to authorize. The more traditional "end to end stapled anastomosis" is a relatively simple operation. The healing time is much shorter than the "J pouch" procedures because there is no hand suturing and no need for a temporary colostomy. The quick healing of the wound also may facilitate the beginning of adjuvant therapy. In addition, you will not have to wear a colostomy bag for three to four months and then have to endure another major surgery to reverse the colostomy.
With all of the negatives related to the J-pouch surgery, you may be asking why would you want to endure these additional problems. It is likely that your surgeon will recommend a J-pouch because he will tell you that the J-pouch will result in better bowel function.
The reality is that the removal of most of your rectum will result in long term bowel functional problems no matter which surgical procedure you have. Without a rectum you will suffer the consequences of rectal removal. There seems to be general consensus that is supported by medical research that there is a perceivable improvement in bowel function immediately after surgery if you have a J-pouch as opposed to an "end-to-end" anastomosis. However, most research shows that the improvement is temporary. The difference in bowel function is about the same within a year.
The question that is very rarely discussed is if the additional expense of treatment, lengthened hospital stay, temporary colostomy, colostomy takedown surgery, increased risk of surgical complications and possible delay of the start of adjuvant therapy is worth the temporary and marginal improvement in bowel function. This is a very hard question to answer. No matter which option you may choose, you will suffer the consequences of the surgery. If you elect to have an "end to end" procedure and then have the predicted poor bowel functions you may immediately regret your decision. However, if you look back on the decision after a year and realize that you are in the same position no matter which procedure you had endured, you may have a different perspective.
Educate Yourself
Surgery A ACS Guide to Surgery for Colon and Rectal Cancer
Surgery for Rectal Cancer General discussion of options
Anterior Resection of the Rectum A good discussion of anterior resection
Ileal Pouch reconstruction Discussion of the Ilea Pouch
Method and Results of Sphincter Preserving Surgery A leading research article from Ireland and France
Surgical Methods of Treatment A French review of the treatment
Explore on Goggle with these key words: Colorectal Cancer, Bowel Cancer, Rectal Cancer Surgery, Colostomy, Anastomosis